Almost every pest control operator has encountered a customer with possible imaginary insect infestations. Smart PCOs refer these clients to a physician.
If they have been in business very long, most PCOs have encountered clients who claim that invisible insects or mites are in or on their skin. For proof, the clients may even bring in tiny bottles, bags, envelopes, etc., containing specks of dust, hair, lint or skin that they claim contain the offending specimens.
In response, the PCO may repeatedly inspect the premises and sometimes even apply pesticides — all to no avail. And, more often than not, the client becomes discouraged with that particular PCO and moves on to another — or even a doctor or university entomologist. Such wandering among PCOs, physicians and entomologists leads to frustration and even hard feelings among all parties involved and may last for years without the patient ever receiving the help he or she really needs.
This condition, called delusions of parasitosis (DOP), is an emotional disorder characterized by an unshakeable belief that tiny, almost invisible insects or mites are living on or in the body. Apparently, DOP is a true delusion and no argument or scientific evidence can convince the patient there is no infestation.
The condition was first recognized by Georges Thibierge in the late 1800s, but the appropriate definition and terminology were not applied until later. It has been called Ekbom’s Syndrome, delusionary parasitosis, delusory parasitosis and others. The most accurate term (in my opinion) is "delusions of parasitosis."
Adverse health effects from DOP include radical patient efforts to rid themselves of the "bugs," such as quitting jobs, burning furniture, abandoning homes and using powerful pesticides dangerously. One man I knew piled all his household furniture in the backyard and burned it. His comment at that time was, "The house is next if this doesn’t get ’em."
WHAT CAUSES DOP? Scientists have studied DOP for years. Careful analysis of DOP cases can provide us with clues about how people develop the illness. The patient is characteristically an elderly female. It has been my experience that younger patients (less than 50 years old) are invariably male.
Most patients have as their main complaint tiny insects or mites crawling under their skin, biting, tickling or burrowing. Seldom is itching the primary complaint. Skin sores and marks may be present, though the patient may have made them by scratching, digging and the like. Other skin damage may be present resulting from intense scrubbing (steel wool, metal scratch pads, etc.) or the use of harsh chemicals, such as gasoline or bleach.
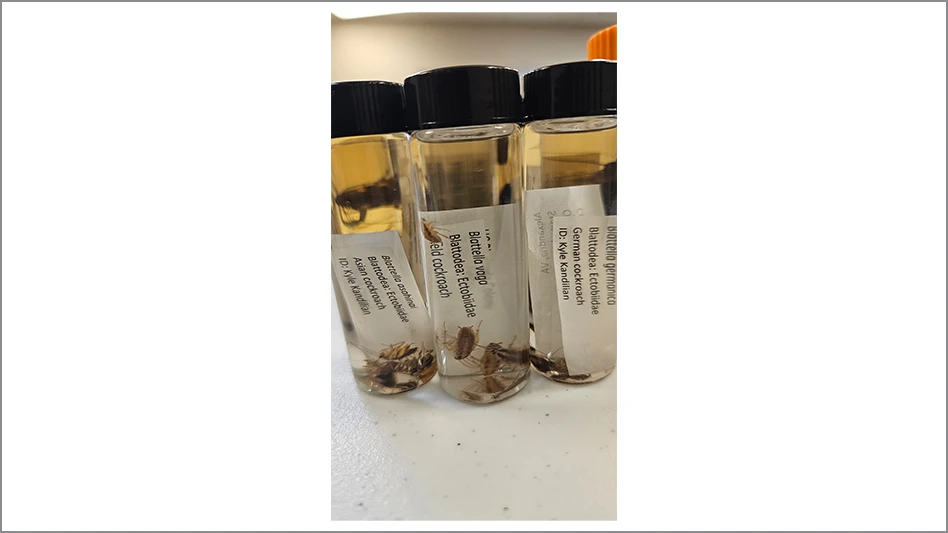
In one study, 82 percent of DOP patients presented with "evidence" of their infestation that included tiny, non-harmful insects, dust, specks of debris and skin or ear scrapings wrapped up in paper, jars or vials. One of the most prominent features of DOP is the client’s absolute conviction that he or she knows exactly what is going on. The client may also be angry that his or her PCO cannot even see, much less eliminate, the "bugs." Interestingly, their story may be so convincing that others in the family also share in the delusion — a folie a deux.
Various events, such as sudden family bereavement, flooding or exposure to parasitized people or animals have been cited as contributing factors. Drug abuse may lead to DOP — one case published in a medical journal was clearly attributed to cocaine use. Sometimes an initial and real insect infestation in the home environment triggers the delusion. For example, if someone with an indoor pet gets fleas inside the home, he or she may still feel mysterious biting long after the fleas have been killed by a PCO.
DISCERNING DOP. First of all, the problem may not be imaginary at all. DOP must be separated from actual insect or mite infestations, as well as from organic conditions that may contribute to a crawling sensation on the skin. Skin scrapings by a dermatologist may be needed to rule out scabies. Sticky traps can be set out in the client’s home and monitored for insects and mites. Samples collected by the client themselves should be examined for the presence of biting insects or mites.
Sometimes a PCO can accomplish this, although a technical services person (some larger pest control companies have a technical service department), local university entomology department or county extension service may be a better alternative. Ideally, the patient’s home should be inspected thoroughly. I know this is labor intensive and PCOs hesitate to do this. Health departments or university personnel sometimes will become involved in home visits, but are under no mandate to investigate private pest problems.
Upon inspection of the house, PCOs should look for bed bugs, rat or bird mites, bat roosts, etc. Sometimes, if there is a bird nest in the wall or rat nest in a couch (or something similar), people may be bitten by parasitic mites. Fortunately, when the nests are found and eliminated, the mites do not take up residence on people (living in their skin, ears or nose).
Keep in mind there may be diseases causing the crawling sensation. This is why DOP clients should be referred to their family doctor. Diabetes, icterus, atopic dermatitis and lymphoblastomas have skin manifestations that can mistakenly be considered arthropod induced. At times, pellagra (caused by a vitamin deficiency) may produce DOP that disappears with appropriate therapy.
WHAT CAN BE DONE? An interdisciplinary approach is needed to help DOP patients, mainly involving family practice physicians, dermatologists, psychiatrists, PCOs and entomologists. Physicians need to be careful not to diagnose "insect bites" based upon skin lesions alone and should call upon entomologists to examine samples. PCOs and entomologists need to understand the medical complexity of delusions — that there are intensive obsessional worries, true delusions and a whole host of abnormal personality traits associated with DOP — and avoid any hint of medical evaluation of the patient.
Although psychiatric evaluation is needed, most DOP patients will not see a psychiatrist (even if referred by a family doctor). Instead, they will seek out another physician or entomologist, thus starting the whole process over again. There is actually a medicine to treat DOP — the antipsychotic drug, Pimozide. Controlled studies (although with few patients) have shown a response rate of about 90 percent to Pimozide. This is all the more reason to try to get your possible DOP clients to go to their doctor.
DOP is a medical condition and the PCO must be careful not to make medical evaluations. Be careful what you tell clients with possible DOP. You could be sued for making statements that defame or cause emotional injury in your client. This is what I do: I gladly look at their samples (collected from their homes, etc.) and then firmly tell them, "This is not a bug. What you have described to me is not caused by any bug I know. It’s not a bug problem. You need to see your family physician."
Editor’s note: PCT has had many requests for a story about DOP and information that pest management professionals can give to their customers about unexplainable itches and bites. The tear-out sheet below has been written by Dr. Jerome Goddard for PCOs to copy and give to their customers who may have additional questions. We have left the top of the hand-out sheet blank so that PCOs can add their name and phone numbers so that their customers can contact them with questions. Feel free to copy this sheet and distribute it to your customers as many times as you like.
Click here for Dr. Jerome Goddard's tear-out sheet (Note: You must have Adobe Acrobat to open this file):
www.pctonline.com/articles/images/delusion_tearout.pdf
The author is a medical entomologist for the Mississippi Department of Health. He can be reached at jgoddard@pctonline.com or 601/576-7512.

Explore the April 2001 Issue
Check out more from this issue and find your next story to read.
Latest from Pest Control Technology
- Bug Busters Expands Service Footprint with New Georgia Branch
- Rodents Can Find Refuge from the Cold in Unused Vehicles
- Natasha Wright Discusses Winter Rodent Habits
- Truly Nolen Promotes Harush, Alvare
- Fleetio Report Finds 53.3% of Fleets Researching or Piloting AI Capabilities
- TRUCE Software Secures Series B Funding
- Richard Spencer Reviews Safety Standards and Training for Technicians
- Kimberly Camera, Canine Team are Hot on Rodent Trails