 Bed bugs affect people in a number of ways, but perhaps the most important are various skin reactions and allergic reactions. True allergic reactions are rare from bed bug bites, and anaphylactic shock is even rarer; however, people often claim that severe bite reactions are allergic (but sometimes this is not the case). The presence of itchy, red bumps, and even blood blisters, are more common. This brief article attempts to classify in laymen’s terms the various reactions resulting from bed bug bites.
Bed bugs affect people in a number of ways, but perhaps the most important are various skin reactions and allergic reactions. True allergic reactions are rare from bed bug bites, and anaphylactic shock is even rarer; however, people often claim that severe bite reactions are allergic (but sometimes this is not the case). The presence of itchy, red bumps, and even blood blisters, are more common. This brief article attempts to classify in laymen’s terms the various reactions resulting from bed bug bites.
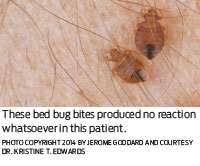
Actually, the most common response to a bed bug bite appears to be no skin reaction at all, with a barely visible tiny hole (punctum) at the location of the bite. Research studies have shown that anywhere from 30 to 60 percent of people bitten by bed bugs have no reaction whatsoever. Common skin reactions for which medical attention is sought are usually 2- to 5-mm itchy red spots at bed bug feeding sites, one per insect. These usually itch, and if not abraded, resolve within a week or so. The size and itchiness associated with these common reactions may increase in some individuals who experience repeated bites. I have known several people who said bed bug bite reactions are extremely itchy.
Complex Skin Reactions.
Some patients may experience complex skin reactions. Reports of these have included itchy wheals (local urticarial or hives) around a central punctum, itchy small red bumps, or diffuse hives at bite sites usually noted or arising in the morning. Blister-like rashes may occur upon new biting events days later. In some cases, these reactions evolve into itchy papules or nodules (hard bumps) that when scratched may become infected (impetiginous) and persist for weeks. These “secondary infections” from scratching bed bug bites can become quite serious and require medical care.
The timing of cutaneous reactions to bed bugs may change with multiple exposures. This appears to reflect host immunological responses to the proteins in bed bug saliva. In other words, the person is becoming more sensitized to the bites each time. One of the original bed bug researchers, Robert Usinger, fed a colony of bed bugs on himself weekly for seven years and noted that his reactions progressed from delayed to immediate, with no evidence of desensitization. The time required for breaking out in a rash got shorter each time due to him becoming more sensitive to the bites.
For another example, one hotel guest noticed isolated macules (flat red spots) after her first visit to a hotel. After a second stay at the same hotel one year later, macules again appeared but this time changed over the next three days into crops of red nodules with blisters. She was skin tested by an allergist with a bed bug salivary gland extract a year after the second hotel stay. Dermal injection of increasing concentrations of the extract resulted in a dose-related increase in the size of the reactions that occurred within 20 minutes of injection. These wheal and flare reactions developed into papular reactions after another 24 hours. The most concentrated salivary solution caused a big papule on her skin with a blister, showing that the reaction was indeed due to substances contained in the bed bug saliva. In more recent research, at least three salivary proteins have been identified that may play a role in these host immunological responses: nitrophorin, a 17-kDa anticoagulant called Factor X and a 40-kDa apyrase-like nucleotide-binding enzyme.

Systemic Allergic Reactions.
There are a few reports of systemic allergic reactions from bed bug bites, for instance asthma, generalized hives and anaphylaxis. Some authors have suggested that generalized (allergic) hives from bed bug bites is not that unusual. One man staying in a hotel awakened during the night with severe itching and hives on his arm and neck; bed bugs were found in the room. He developed what appeared to be some sort of anaphylactic shock, was hospitalized and had transient anterolateral ischemia on electrocardiogram (it appeared he had a heart attack). Eight months later, after an experimental bed bug bite in the clinic, he developed a wheal at the bite site and generalized itching severe enough to require epinephrine administration to resolve his symptoms. A home evaluation of another man who had asthma revealed bed bugs in his bedding and an intradermal allergy skin test with an extract of bed bugs showed positive results. When his bedding was changed, the asthma attacks ceased.
Only physicians should give medical treatment advice. Treatments of common and complex cutaneous reactions are usually just symptomatic, aimed at relieving inflammation and itching. Typically physicians recommend that bite sites be washed with soap and water to help prevent secondary infection. If skin lesions are severely itchy, they often suggest topical application of over-the-counter or prescription anti-itch medications or intermediate potency corticosteroids (such as triamcinolone) may be helpful. Sites that appear to be secondarily infected may benefit from topical antibiotic creams or systemic antibiotics as appropriate.
Goddard is the author of “The Physician’s Guide to Arthropods of Medical Importance.” He is an extension professor of medical and veterinary entomology at Mississippi State University.

Explore the December 2014 Issue
Check out more from this issue and find your next story to read.
Latest from Pest Control Technology
- SiteOne Hosts 2024 Women in Green Industry Conference
- Veseris Celebrates Grand Reopening of the Miami ProCenter
- Rollins' 2024 Second Quarters Revenues up 8.7 Percent YOY
- Fleetio Go Fleet Maintenance App Now Available in Spanish
- German Cockroach Control Mythbusting
- Total Pest Control Acquires Target Pest Control
- NPMA Workforce Development Shares Hiring Updates
- Certus Acquires Jarrod's Pest Control





